Uterine fibroids are a common women’s health concern, affecting millions of people during their reproductive years. While these noncancerous growths are almost always benign, they can cause a range of symptoms that impact quality of life. Understanding the different types of fibroids and where they grow in the uterus can help you make informed decisions about treatment options. We’ll explore the four main types of uterine fibroids: intramural, subserosal, submucosal, and pedunculated, and discuss how they differ, where they’re located, and the symptoms they may cause, helping you recognize when it’s time to seek expert care.
Types of Fibroids
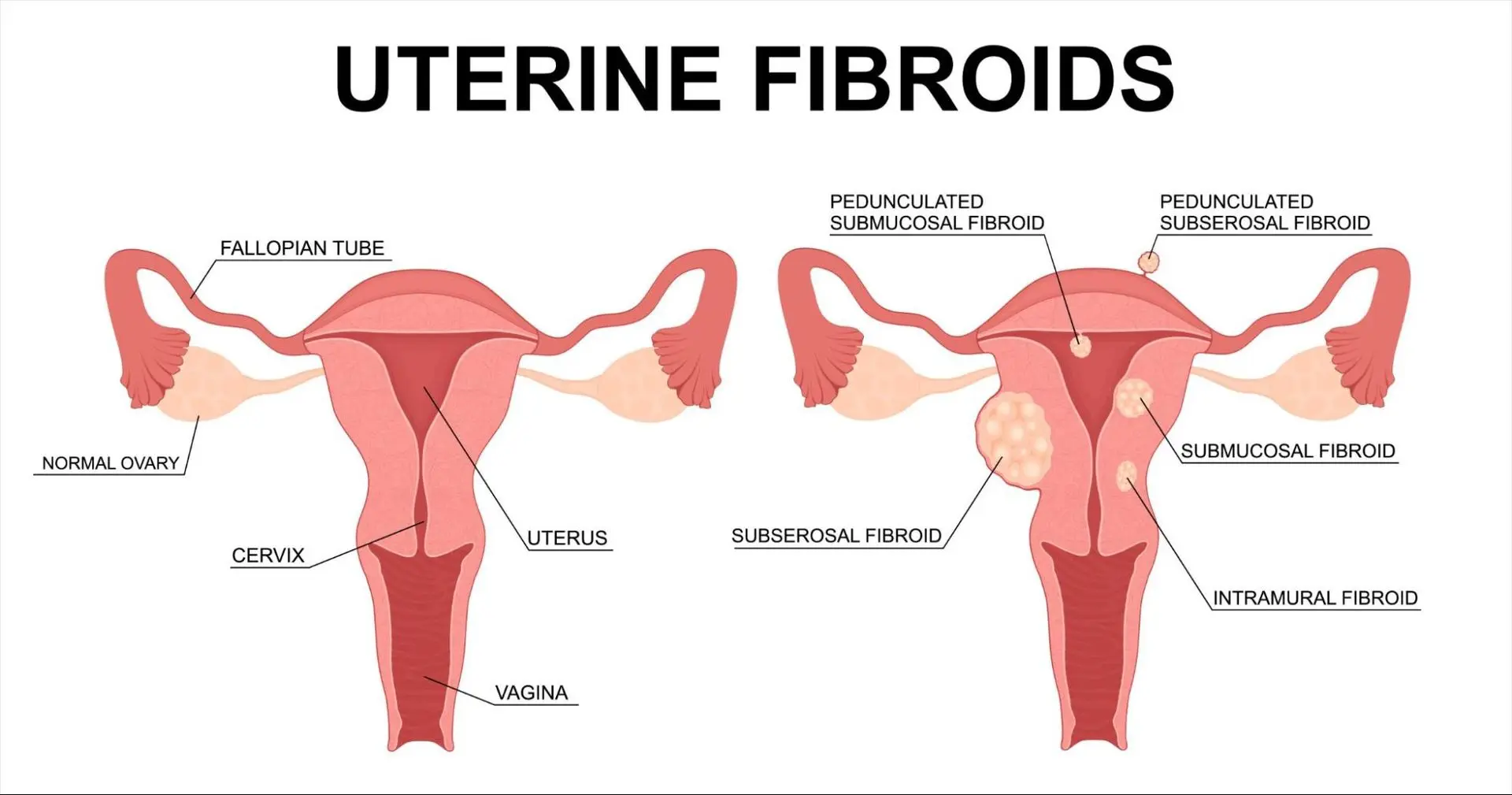
Fibroids, also known as leiomyomas or myomas, are classified based on their location in the uterus. The four primary types are:
- Intramural fibroids
- Submucosal fibroids
- Subserosal fibroids
- Pedunculated fibroids
Each type can behave differently: for example, submucosal fibroids are most likely to affect fertility because of their location near the uterine cavity, while sub-serosal fibroids generally have less impact on getting pregnant. Fibroids are also dynamic: they often grow under the influence of estrogen and progesterone. Some fibroids grow during pregnancy and may then shrink or “degenerate” afterward. Let’s start by focusing on the details and the symptoms for each.
Intramural Fibroids
Intramural fibroids are the most common type of uterine fibroid. They develop within the muscular wall (myometrium) of the uterus. As they grow, intramural fibroids can cause the uterus to appear larger than normal, sometimes leading to a sensation of pelvic fullness or pressure.
Symptoms of Intramural Fibroids:
- Heavy or prolonged menstrual bleeding
- Pelvic pain or pressure
- Frequent urination (if the fibroid presses on the bladder)
- Lower back pain
Because intramural fibroids are embedded in the uterine wall, they can sometimes distort the shape of the uterus, potentially affecting fertility or pregnancy, especially if they become large.
Subserosal Fibroids
Subserosal fibroids grow on the outside of the uterus, just beneath the outermost layer called the serosa. These fibroids can extend outward into the pelvic cavity. Subserosal fibroids are less likely to cause heavy menstrual bleeding but are more likely to cause symptoms related to pressure on surrounding organs.
Symptoms of Subserosal Fibroids:
- Pelvic pain or discomfort
- Pressure on the bladder, leading to frequent urination
- Pressure on the rectum, causing constipation
- Abdominal distension or a feeling of fullness
Because subserosal fibroids grow outward, they can become quite large before causing noticeable symptoms. In some cases, a large subserosal fibroid can be felt as a firm mass in the lower abdomen.
Submucosal Fibroids
Submucosal fibroids are less common but can cause the most significant symptoms. These fibroids develop just beneath the lining of the uterine cavity (endometrium) and can protrude into the uterine cavity itself.
Symptoms of Submucosal Fibroids:
- Heavy, prolonged, or irregular menstrual bleeding
- Passing blood clots during menstruation
- Anemia due to excessive blood loss
- Fertility problems or recurrent pregnancy loss
Because submucosal fibroids disrupt the uterine lining, they are most closely associated with abnormal uterine bleeding and can interfere with embryo implantation, making conception more difficult.
Pedunculated Fibroids
Pedunculated fibroids are unique because they grow on a slender stalk that connects them to the uterus, rather than developing directly from the uterine wall. When a pedunculated fibroid forms on the outer surface of the uterus, it is called a pedunculated subserosal fibroid and extends outward into the pelvic cavity. If the fibroid develops on a stalk just beneath the uterine lining, it is known as a pedunculated submucosal fibroid and protrudes into the uterine cavity
Symptoms of Pedunculated Fibroids:
- Pelvic pressure or discomfort
- Sudden, sharp pelvic pain (if the stalk twists, a condition called torsion)
- Symptoms similar to their subserosal or submucosal counterparts
Pedunculated fibroids can sometimes be mistaken for ovarian masses during imaging, and their stalks make them more prone to acute pain if they twist.
How Fibroids Can Affect Fertility
Many women with fibroids have no trouble conceiving or carrying a baby. “Yes, many patients with fibroids can get pregnant,” affirm fertility specialists. However, fibroids can interfere with fertility in certain situations. It all depends on their size, number, and especially location. In particular:
- Implantation interference. Submucosal fibroids (those bulging into the uterine cavity) can change the shape of the uterus and make it harder for an embryo to implant in the lining. As Dr. April Milan Miller of Wake Forest Baptist explains, “submucosal fibroids can distort the shape of the uterine cavity and make it difficult for a fertilized egg to implant”.
- Blockage of tubes. A large fibroid near the entrance of a fallopian tube can physically block the tube, preventing an egg and sperm from meeting. Although this is uncommon, it can occur if a fibroid is located at the uterine cornua.
- Impaired blood flow. Very large fibroids may reduce blood flow to the uterine lining, potentially impairing the environment needed for implantation.
- Inflammatory or hormonal effects. Fibroids may create subtle changes in uterine hormones or inflammation (though research is ongoing on this point).
Studies show fibroids are found in 5–10% of women evaluated for infertility, and fibroids alone are thought to be the sole cause of infertility in only about 1–2% of cases. In other words, most women with fibroids do conceive; yet fibroids can contribute to difficulty, especially when other fertility issues are present. “Fibroids are one of many things that can impact fertility,” notes Dr. Miller, so it’s important to have a thorough work-up. Gynecologists therefore recommend that women trying to conceive discuss fibroids with their doctor, especially if they have recurrent pregnancy loss or unexplained infertility.
Fibroids and Pregnancy
Once pregnant, many women with fibroids go on to have healthy pregnancies. However, fibroids can raise certain pregnancy risks. The specific risks depend on how big the fibroids are and where they are. Doctors have observed that fibroids may be associated with:
- Miscarriage and preterm labor. Women with multiple or large fibroids have a slightly higher risk of pregnancy loss and early delivery. (The exact increase is modest, but it is significant especially if fibroids are numerous or submucosal.)
- Malpresentation and cesarean delivery. Fibroids can prevent the baby from settling into a head-down position, raising the chance of breech birth. In fact, pregnant women with fibroids are about six times more likely to need a cesarean section than those without.
- Placental complications. Placenta previa or placental abruption can occur more often if fibroids distort the uterus.
- Pain and bleeding. As pregnancy progresses, fibroids may outgrow their blood supply and degenerate, causing acute pain (often in the second or third trimester). They can also contribute to vaginal bleeding or placental issues.
- Other issues. There may be a slightly higher chance of postpartum hemorrhage (heavy bleeding after birth) and labor dystocia if fibroids are present.
Despite these risks, most fibroid-related pregnancy complications can be managed. We advise close monitoring with ultrasounds, and sometimes the involvement of a high-risk obstetrician if needed. Importantly, fibroids themselves are not removed during pregnancy except in very rare, emergency circumstances. If symptoms are severe, we manage them with conservative measures (hydration, pain relief, bed rest as needed) until after delivery.
Diagnosing Fibroids
Fibroids are often detected during a routine pelvic examination or an early pregnancy ultrasound. When symptoms such as heavy menstrual bleeding, pelvic pressure, or pain raise suspicion, the next step is to confirm their presence through imaging.
Ultrasound—either transvaginal or abdominal—is usually the first test. It helps determine the size, number, and location of fibroids.
For patients undergoing a fertility evaluation, tests like a hysterosalpingogram (HSG) or sono-hysterogram are commonly used to assess the uterine cavity and fallopian tubes.
If an ultrasound does not provide enough clarity, an MRI can offer a more detailed and comprehensive view of the uterus. In certain situations—especially when fibroids may be contributing to infertility—procedures such as diagnostic hysteroscopy or laparoscopy may be recommended to directly visualize the uterus, fallopian tubes, and ovaries.
A complete fertility assessment is essential. If you have fibroids and are unable to conceive within 6–12 months (or earlier if you are older), consulting a reproductive endocrinologist is advised. This helps rule out other potential causes of infertility before linking the difficulty solely to fibroids.
Treatment Options (Preserving Fertility)
Not every fibroid needs treatment. If your symptoms are mild and your daily life is unaffected, I usually suggest simple monitoring. However, if fibroids cause heavy bleeding, pain, or are affecting fertility, there are several fertility-friendly options:
1. Medications for symptoms
Pain relievers like ibuprofen can ease cramps. Hormonal methods or a levonorgestrel IUD can reduce heavy bleeding, and tranexamic acid helps control flow during periods. These treatments don’t shrink fibroids but can make symptoms manageable while you plan pregnancy or surgery. (Hormonal options must be stopped before trying to conceive.)
2. Temporary fibroid-shrinking medicines
GnRH agonists/antagonists can shrink fibroids for a short time—often used before surgery to make removal easier. Once the medicine stops, fibroids tend to grow back, so these are not long-term solutions for fertility.
3. Myomectomy (fibroid removal)
This is the best surgical option for women who want to preserve fertility. Depending on fibroid size and location, it can be done:
- Hysteroscopically (through the vagina, no cuts on the abdomen)
- Laparoscopically (small incisions)
- Open surgery (for very large or multiple fibroids)
The uterus is repaired carefully, and I usually advise waiting 3–6 months before trying to conceive. Many women successfully get pregnant after a myomectomy.
4. UFE and other procedures
Uterine Fibroid Embolization and MRI-guided procedures can shrink fibroids, but since their fertility outcomes aren't well-established, I rarely recommend them for women trying to conceive soon.
5. Hysterectomy
This is the only permanent cure but removes the uterus entirely. I reserve this option only for women who have completed their family or have severe, unmanageable symptoms.
Tips for Trying to Conceive with Fibroids
Based on both evidence and clinical experience, here are some practical tips and advice:
• Early evaluation. If you have fibroids and wish to become pregnant, discuss this with your doctor early. Be open about your fertility goals so they can guide you. “Talk to your healthcare provider about your fertility goals when discussing treatment options,” advises the Cleveland Clinic. Many patients benefit from seeing a fertility specialist (reproductive endocrinologist) especially if conception is difficult.
• Monitor fibroids. Regular ultrasounds can track fibroid growth. Fibroids tend to grow over time under hormonal influence, so delaying pregnancy can sometimes mean bigger fibroids later. One study noted fibroids are far more common in women over 40 than in their 20s. If you are older or have multiple fibroids, discuss timing of pregnancy and treatment sooner rather than later.
• Consider fertility preservation. If a fibroid removal surgery is recommended but you’re not ready to conceive immediately, discuss egg or embryo freezing. Fertility preservation allows you to maintain options. For instance, UChicago Medicine suggests freezing eggs if fibroid treatment might affect fertility.
• Address anemia. Heavy bleeding from fibroids can cause iron deficiency. If you have anemia, taking iron supplements can improve your health and fertility. Many gynecologists routinely check iron levels in women with fibroids. Treating anemia ensures you’re in the best shape to conceive and support a pregnancy.
• Healthy lifestyle. While fibroids have a strong genetic and hormonal basis, general health matters too. Maintaining a healthy weight (high BMI can increase fibroid risk), eating a balanced diet rich in fruits and vegetables, and getting regular moderate exercise may help control fibroid growth and improve fertility. Likewise, managing stress and chronic conditions (like thyroid issues or high blood pressure) optimizes fertility overall.
• Symptom management. If fibroids cause pain or pressure, talk to your doctor about pain-relief options. Some women find relief with heat therapy, gentle exercise, or yoga. If daily activities are affected, Dr. Miller advises scheduling an OB/GYN appointment promptly. Don’t ignore worsening symptoms; better to address them early.
• Stay informed. Advances in fibroid treatment continue. For example, new medications are emerging to control bleeding, and minimally invasive surgeries have become safer. As an experienced gynecologist, I encourage patients to ask questions, get second opinions if needed, and choose a care team experienced in fibroid management.
Takeaway from Dr. Madhu Singh
After more than three decades of caring for women with fibroids, my message is simple: fibroids are common, treatable, and many women with fibroids go on to have healthy pregnancies. What matters most is understanding the type, size, and location of your fibroids and choosing a treatment plan that aligns with your symptoms and fertility goals.
Not every fibroid needs treatment—sometimes careful monitoring is enough. When symptoms do affect daily life or fertility, we have several safe, effective, and fertility-preserving options. Early evaluation, regular follow-ups, and honest conversations about your pregnancy plans can make a meaningful difference.
Most importantly, listen to your body. If something feels off—pain, heavy bleeding, difficulty conceiving—seek care early. With the right guidance and timely treatment, you can protect your health, your uterus, and your future fertility.
— Dr. Madhu Singh, OB/GYN