Many women suffer silently with endometriosis for years before getting help. What starts as severe period cramps or pelvic pain can become a constant burden on daily life and mental health. Endometriosis is a chronic condition in which tissue similar to the uterine lining grows outside the uterus. It often causes debilitating pain, heavy bleeding, fatigue, and infertility, affecting roughly 1 in 10 women of reproductive age. Without a cure, persistent pain can lead to long-term physical and emotional complications that severely reduce quality of life. In other words, living years with undiagnosed endometriosis means enduring needless suffering.
What the Research Shows :
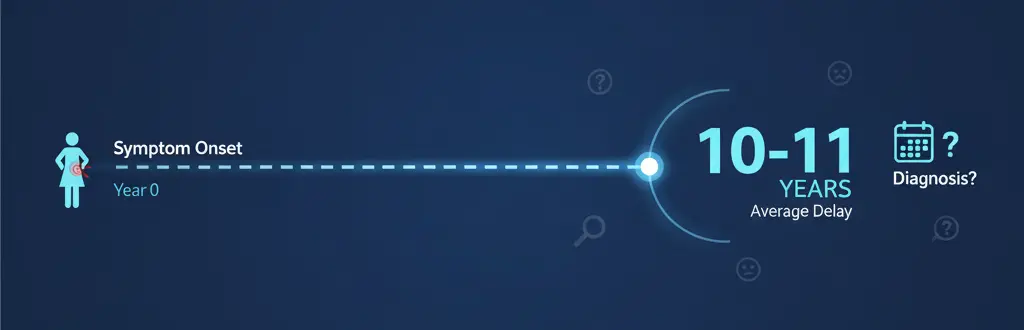
Long delays are common. Studies consistently report that women wait many years to be diagnosed. For example, one review found women often wait up to 10–11 years from symptom onset to diagnosis. Many see multiple doctors (an average of 5 visits) before a specialist suspects endometriosis. These delays mean more time spent in pain and uncertainty.
Delays worsen outcomes. Research shows that long diagnostic delays let the disease progress. Reviews link delays to increased symptom severity, fertility problems, and rising emotional distress. For instance, one analysis noted that delays contribute to “disease progression, higher likelihood of fertility problems, significant patient distress and the need for more complex intervention”. In practical terms, each extra year without diagnosis can mean more scar tissue, heavier treatment, and harder recovery.
Quality of life suffers. Endometriosis affects every aspect of life. Systematic reviews highlight chronic pain, infertility, and mood symptoms (anxiety, depression) as major burdens. The long wait for answers adds frustration and isolation: one review reports that “long time required to diagnose leads to frustration and isolation and increases psychological distress, shame, anxiety, and depressive symptoms”. In short, women often endure not only physical pain but also mental strain from feeling disbelieved or misunderstood.
Early treatment helps – even if diagnosis was delayed. Importantly, studies show that women’s quality of life improves after effective treatment, no matter when they get diagnosed. In a recent clinical study, both early-diagnosed and late-diagnosed patients saw significant Quality of Life gains after 18 months of treatment. This means that once the disease is identified, medical or surgical therapies can bring relief. However, researchers still stress that preventing years of suffering is preferable. Early diagnosis allows simpler interventions and preserves fertility options. One expert review concluded that endometriosis care should prioritize “early diagnosis and initiation of effective treatment to prevent emotional distress associated with delayed diagnosis”.
Awareness is low, so education is crucial. Studies and expert commentators emphasize the need for public and provider education. For example, an obstetrician from Rutgers Health notes that “lack of knowledge of the disease combined with stigma causes an average delay of 10 years from onset of symptoms to diagnosis”. Around half of people have never heard of endometriosis, and many who have cannot name any symptoms. As one review puts it, we must combat the normalization of pain with targeted education about endometriosis. In short, raising awareness at schools, clinics and in the media is shown to be a key step toward earlier care.
A Gynecologist’s Perspective :

In my own practice, I regularly meet women who have endured years of pain with no diagnosis. Most describe being told “this is normal” or simply taking painkillers from a young age. Unfortunately, that messaging is common : patients often learn (sometimes from family or cultural taboos) that heavy periods are just part of being a woman. Research confirms this pattern : many women say their pain was dismissed by doctors or relatives, forcing them to push for a referral before anyone took them seriously.
I always tell my patients that their pain is real and important. Endometriosis isn’t “all in your head.” In fact, chronic inflammation from this disease can cause systemic effects – things like fatigue, headaches and mood swings – that patients frequently report. One recent review noted that many women with endometriosis also suffer from “fatigue and sleep disturbances,” likely related to inflammation and chronic pain. These symptoms often worsen anxiety and depression, creating a vicious cycle.
Because of these complexities, I stress open communication : I encourage women to keep track of their symptoms and insist on answers if something feels off. The evidence backs this up – experts call for better education so that neither patients nor doctors normalize debilitating pain. For instance, many women feel “vindicated” and relieved once they finally receive a diagnosis and name for their pain. This validation matters: it helps patients feel supported and makes a difference in mental well-being. Ultimately, I’ve seen again and again that when endometriosis is recognized early, we can move faster to treat it and restore quality of life.
Practical Tips & Advice :
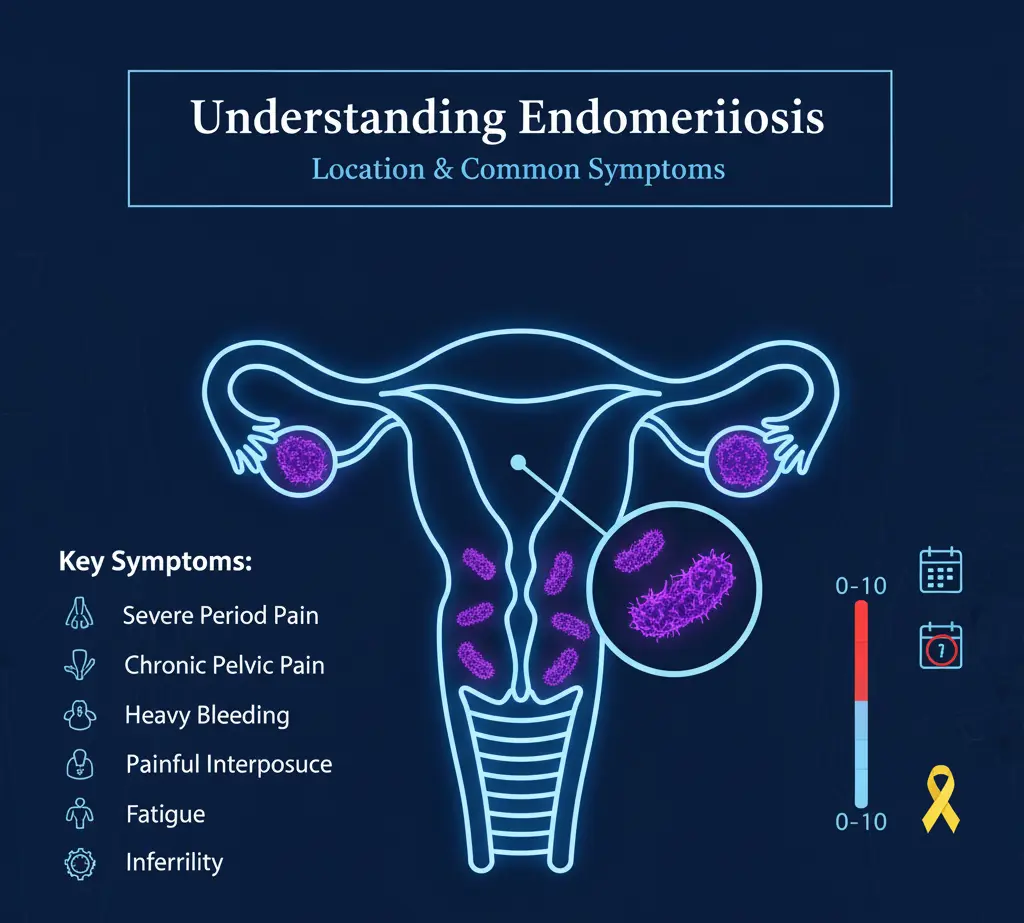
Key symptoms to watch for: Severe period cramps (dysmenorrhea), chronic pelvic pain (not just “during” but between periods), heavy or irregular menstrual bleeding, pain during intercourse, and pain with bowel movements or urination during periods are red flags. Some women also have longstanding fatigue, headaches or digestive issues that worsen around their cycle. If these symptoms disrupt your daily life or school/work, they should not be ignored.
See a gynecologist early: If menstrual pain is so bad that over-the-counter meds don’t help, or if you’ve seen your doctor multiple times without relief, ask for a referral to a specialist. Many guidelines suggest seeking specialty care if you suspect endometriosis or if period pain is disabling. (This is especially true if you’re also concerned about fertility – up to 50–70% of women evaluated for infertility or chronic pelvic pain have endometriosis.) An OB/GYN can evaluate you and discuss options like imaging tests or a diagnostic laparoscopy if needed.
Track your symptoms: Keep a simple diary or use an app. Note the intensity and timing of your pain, bleeding, bowel symptoms and fatigue. This record helps your doctor see patterns. Research shows that even patient-reported symptom questionnaires can speed up diagnosis. Providing objective details (e.g. “pain level 8/10 on day 2 of period”) can make a big difference in getting a proper evaluation.
Talk openly about menstrual health: Break the taboo. Share your experiences with friends or family you trust. You might be surprised how many women struggle with the same issues. Support groups, online communities or endometriosis foundations can be helpful. Educate others that severe period pain is not “normal.” Healthcare providers are also listening more now – more education means they will take your concerns seriously.
Plan for the future: If you’re planning a family, remember that endometriosis can affect fertility. Early intervention can preserve fertility options. Discuss with your doctor any concerns about conception; in many cases, timely treatment improves chances of pregnancy.
Q: Is endometriosis curable? Currently, there is no known cure for endometriosis.
Treatments (medications, hormonal therapy, and surgery) can manage symptoms and improve life quality, but they work best when started early. Managing pain and preventing complications is the goal of treatment.
Q: Can endometriosis cause fatigue?
Yes. Many women with endometriosis experience chronic fatigue, brain fog, or sleep problems. Medical reviews note that endo-related inflammation and chronic pain can disrupt sleep and energy levels. Addressing endometriosis (and related anemia or sleep issues) often helps improve fatigue.
Q: Does early diagnosis make a difference?
Absolutely. Early diagnosis can change lives by shortening the years of pain before treatment. As one expert put it, “receiving an early diagnosis and treatment… can have a major impact for patients”. Even if symptoms are mild at first, identifying endometriosis early allows you to intervene (with medication or minimally invasive surgery) before the disease worsens.
Take Action :
Endometriosis is not something you should have to “tough out” alone. If your symptoms are affecting your life – physically or emotionally – seek help. Talk openly about menstrual pain with your loved ones and healthcare provider. Educate yourself (and them) with reliable information. Early awareness and diagnosis are key to preserving quality of life.
As a gynecologist, I tell my patients: you deserve answers and relief. No one should normalize suffering. If you suspect endometriosis in yourself or a loved one, please book a consultation or reach out to a women’s health specialist. Remember, early diagnosis isn’t just a medical step – it’s the first step toward feeling better and taking back control of your health.
Remember:
Menstrual pain is common, but it shouldn’t control your life. By raising awareness and acting on symptoms early, we can change outcomes for countless women. As one advocate wisely said, “Awareness is the first step toward healing. No woman should have to normalize pain.”